Health Equity
Medicaid Enrollment Touches 39% of the Residents of The District of Columbia; DC’s 70/30 FMAP is Vital for the Maintenance of Health & Human Services
A reduction in the District’s FMAP would not lead to long-term government savings and would have a ripple effect throughout the entire health system in the DMV, crippling access to care for not only Medicaid beneficiaries but also all those who live, work, and visit the District of Columbia, including members of Congress and their staffs.
.png?sfvrsn=9ac2d21b_0)
Why does DC receive an Enhanced FMAP Rate?
The DC FMAP rate of 70% established by the Revitalization Act resulted from bipartisan analysis, discussion, and negotiation by Congressional leadership aiming to balance fairness with the District’s restricted ability to generate revenue. Congress recognized that the District of Columbia faces unique financial challenges due to its non-state status and the significant amount of federally-owned land within its boundaries. The District is unable to tax non-residents’ earnings, so these workers pay no taxes to support the infrastructure and services, such as roads, public safety and emergency services that they benefit from in the District. The District is also unable to tax up to 40% of the real property within its borders due to statutory restrictions.
Why are we concerned about DC's FMAP now?
Members of Congress have proposed reducing the DC FMAP to the statutory minimum for all other states, which is currently 50% (but could be reduced even more). Such a change would impact every physician and every practice, regardless of type, location, and payers contracted. Even practices who take no insurance will not be able to send patients for specialist care, hospital admissions, or other types of care.
What can MSDC members do?
- If you know a member of Congress or staffer, reach out to them and share how DC cuts will hurt your patients.
- Share your relationships and outreach with hay@msdc.org so we can help coordinate advocacy efforts.
- Email hay@msdc.org if you would like to be paired with a physician member of Congress office and trained by MSDC staff on how to reach out.
Resources
- DC FMAP cut fact sheet
- California Medical Association fact sheet on Medicaid cuts
- MSDC and healthcare association letter to Congress arguing against DC FMAP changes.
- MSDC original story on Medicaid changes.
News, Statements, and Testimony on Health Equity Issues
MSDC President Testifies at DHCF Oversight Hearing
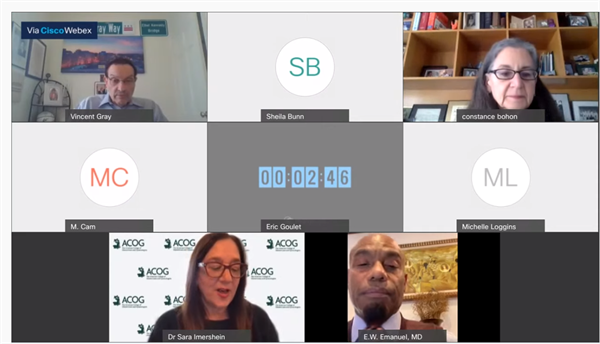
On Thursday, MSDC President Dr. EW Emanuel testified at the Committee on Health oversight hearing for the Department of Health Care Finance (DHCF), Deputy Mayor for Health and Human Services, and United Medical Center.
DC Council committees hold oversight hearings for all District executive agencies as part of the budget process. The committees use the feedback from the hearings to guide budget decisions as well as craft legislation for the year.
Dr. Emanuel testified along with Dr. Sara Imershein and Dr. Connie Bohon, who represented ACOG at the hearing. Dr. Emanuel's written testimony is below.
March 4, 2021
Councilmember Vincent Gray
Chair, Committee on Health
1350 Pennsylvania Ave NW
Washington, DC 20004
Dear Chair Gray,
Thank you for allowing me to testify today at the oversight hearing. My name is E.W. Emanuel, and I am the 2020-2021 President of the Medical Society of DC (MSDC). MSDC is the largest medical organization representing metropolitan Washington physicians in the District. We advocate on behalf of all 11,000 plus licensed physicians in the District and seek to make the District “the best place to practice medicine”.
Medicine is changing in the District and thanks to you and your colleagues, much of it is changing for the better. Your leadership helped bring to fruition the new hospital at St. Elizabeth’s campus, and MSDC is excited to have members at the facility when it opens in the coming years.
However, the public health emergency has made clear the horrendous inequities in the healthcare system. The District has near universal health coverage and world-class medical facilities, but the District still needs to ensure every resident has access to a family physician practice to ensure the best care.
I want to begin by applauding Deputy Mayor Wayne Turnage, Medicaid Director Melisa Byrd, and the entire leadership team and staff of the Department of Health Care Finance. Their work ensured that District residents had access to coverage during the public health emergency. We specifically want to thank the Department of Health Care Finance for their expansion of telemedicine reimbursement early in the public health emergency. Reimbursing visits without seeing patients in-person allowed many residents to receive necessary care.
Looking ahead, I encourage the Committee, Council, and Department to address some looming healthcare issues. We need to ensure that post-COVID we have a robust healthcare network that protects all District residents. To do this I make the following recommendations for the physician community:
1. Protect and promote local physician practices in Wards 5, 7, and 8. World class hospitals are important for the District, but residents need local physician practices to ensure their long-term wellbeing. Unfortunately, financial pressures and financial incentives from Prince George’s County make it harder for physicians to open and maintain practices in the District. A diverse payer mix plus competitive reimbursement rates for Medicare will go a long way to ensuring physicians can open community practices and treat patients where they live.
2. Allow for affiliation agreements with the new hospital. MSDC advocated for the new hospital on the campus of St. Elizabeth’s. Related to the previous point, independent practices need access to the hospital. Moving forward, the District and UHS should not prevent non-UHS or non-GW practices from signing affiliation agreements. Independent practices have agreements with other local hospitals for admitting privileges, and the new hospital should have the same.
3. Fund innovation. MSDC thanks the department for funding initiatives such as the Integrated Care Technical Assistance program that helps practices with technology concerns. We urge the Council to continue funding such initiatives to make the District an attractive place to create a physician practice.
4. Fund the Postpartum Coverage Act of 2019. MSDC agrees with ACOG that L23-132 deserves full funding in this budget to ensure postpartum benefits are fully extended to Medicaid patients.
Please reach out to the MSDC office if I or our membership can be of assistance on this or any issue. We look forward to working with you and the Committee to make the District the best place to practice medicine.
Sincerely,
EW Emanuel, MD

Leave a comment